Endoscopy is required when doctors need to examine the interior of hollow organs or body cavities to diagnose medical conditions, investigate symptoms, perform biopsies, or carry out therapeutic interventions.The procedure involves inserting a flexible tube with a camera and light source through natural body openings, providing real-time visualization of internal structures that cannot be adequately assessed through external examination or imaging alone.
Medical professionals recommend endoscopy when patients experience persistent unexplained symptoms, have abnormal test results requiring confirmation, need screening for diseases, require monitoring of known conditions, or need minimally invasive treatments. The procedure offers unparalleled diagnostic accuracy while minimizing patient discomfort and recovery time compared to traditional surgical exploration.

About Author Dr. Neelakanth Parappanavar – Consultant in Medical Gastroenterology, Expert in Gastro, Liver & Endoscopy
Author of this article Dr. Neelakanth Parappanavar brings extensive expertise as a Consultant in Medical Gastroenterology with specialized training in gastrointestinal disorders, liver diseases, and advanced endoscopic procedures. With years of clinical experience performing thousands of diagnostic and therapeutic endoscopies, Dr. Parappanavar has developed comprehensive knowledge of when endoscopic evaluation becomes medically necessary and how to optimize patient outcomes.
His expertise encompasses the full spectrum of endoscopic procedures, from routine diagnostic examinations to complex therapeutic interventions including polypectomy, variceal banding, stricture dilation, and endoscopic ultrasound. Dr. Parappanavar’s patient-centered approach emphasizes thorough pre-procedural consultation, meticulous technique during examination, and comprehensive post-procedure care.

Conditions When Endoscopy Is Required
Endoscopy becomes medically necessary under numerous clinical circumstances where direct visualization of internal structures provides critical diagnostic information or enables therapeutic intervention. Understanding when endoscopy is required helps patients appreciate why their physician has recommended this procedure.
Persistent Digestive Symptoms: When patients experience ongoing abdominal pain, difficulty swallowing, persistent heartburn, or unexplained nausea and vomiting lasting beyond several weeks, endoscopy is required to identify the underlying cause.
Gastrointestinal Bleeding: Any evidence of bleeding, vomiting blood, passing black tarry stools, or blood in stool makes endoscopy urgently required. The procedure locates the bleeding source and often allows immediate treatment.
Screening for Cancer: Endoscopy is required for cancer screening in individuals with risk factors including family history, previous polyps, inflammatory bowel disease, or Barrett’s esophagus. Regular surveillance enables early detection when cancers are most treatable.
Unexplained Weight Loss: Significant unintentional weight loss often necessitates endoscopy to exclude malignancies, malabsorption disorders, or chronic inflammatory conditions affecting the digestive tract.
Chronic Anemia: When patients have iron-deficiency anemia without obvious external bleeding sources, endoscopy is required to identify occult gastrointestinal bleeding from ulcers, vascular malformations, or tumors.

Types of Endoscopy Procedure
The two primary categories of gastrointestinal endoscopy are upper and lower endoscopy, each addressing different segments of the digestive tract. Types of endoscopy tests extend beyond these to include capsule endoscopy, enteroscopy, ERCP, endoscopic ultrasound, and bronchoscopy. The selection depends on symptoms, suspected diagnosis, and treatment goals.
Upper Endoscopy Procedure
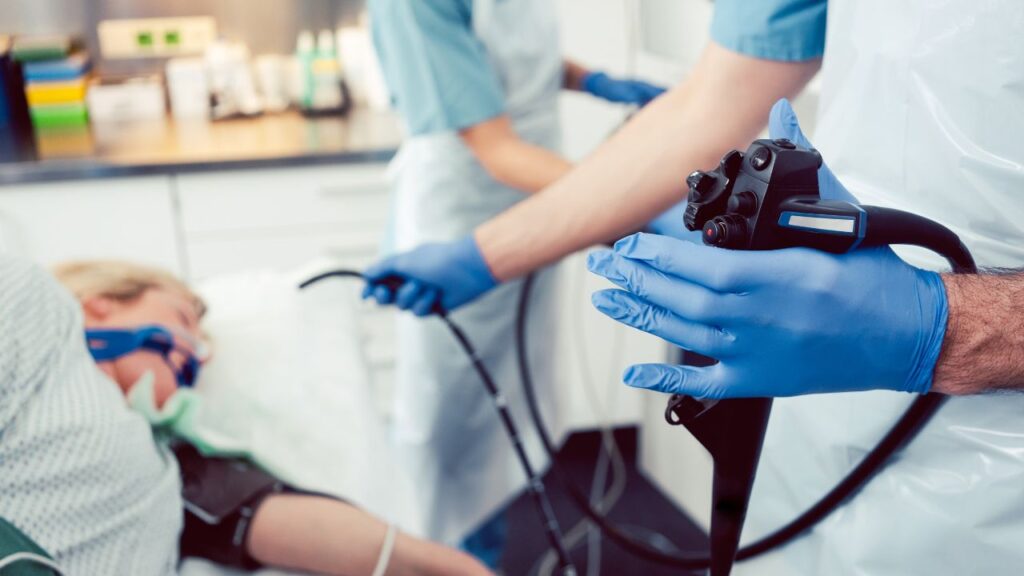
Upper endoscopy (esophagogastroduodenoscopy or EGD) is required when physicians need to examine the esophagus, stomach, and duodenum. The procedure involves passing a flexible endoscope through the mouth and throat into the esophagus, containing a light source and high-definition camera transmitting real-time images.
During upper endoscopy, physicians perform biopsies by passing tiny forceps through the endoscope to collect tissue samples. These samples help diagnose H. pylori infections, Barrett’s esophagus, dysplasia, cancer, and inflammatory conditions.
Upper endoscopy is specifically required for evaluating heartburn unresponsive to medication, difficulty swallowing, persistent upper abdominal pain, suspected ulcers, iron deficiency anemia, and screening for varices in liver disease patients. The procedure takes 15-30 minutes under conscious sedation.
Therapeutic interventions include treating bleeding ulcers, dilating esophageal strictures, removing polyps, banding varices, removing foreign objects, and placing feeding tubes.
Lower Endoscopy Procedure
Lower endoscopy (colonoscopy) is required for examining the entire colon and rectum. The flexible colonoscope is inserted through the anus and advanced through all colon segments. The endoscopist examines all surfaces while slowly withdrawing the instrument.
Lower endoscopy is required for colorectal cancer screening beginning at age 45, investigating rectal bleeding, evaluating chronic diarrhea or constipation, diagnosing inflammatory bowel disease, monitoring known IBD or previous polyps, and investigating unexplained abdominal pain.
During colonoscopy, polyp removal (polypectomy) can be performed immediately when polyps are identified, eliminating precancerous growths before cancer develops. The procedure requires extensive bowel preparation and takes 30-60 minutes under sedation.
How Is an Endoscopy Procedure Done
Understanding how endoscopy procedures are performed helps alleviate patient anxiety and ensures cooperation for optimal examination quality. While specific steps vary between upper and lower endoscopy, both follow systematic protocols prioritizing patient safety, diagnostic accuracy, and procedural comfort.
Pre-Procedure Assessment: Patients undergo medical history review, medication reconciliation, and risk assessment. The gastroenterologist discusses the procedure’s indication, obtains informed consent, and addresses questions.
Sedation Administration: Most procedures are performed under conscious sedation for patient comfort. An IV line is established, and sedative medications are administered. Vital signs are continuously monitored throughout.
Upper Endoscopy Technique: Patients lie on their left side with a mouth guard protecting teeth. The physician advances the endoscope through the mouth, and patients swallow to facilitate passage. Air insufflation expands the stomach for comprehensive visualization. The physician systematically examines all areas, photographing abnormalities and obtaining biopsies.
Lower Endoscopy Technique: The lubricated colonoscope is inserted through the anus. The gastroenterologist advances the scope through the colon using air or carbon dioxide insufflation. Upon reaching the cecum, the physician begins slow withdrawal, meticulously examining for polyps or abnormalities.
Recovery: Patients recover as sedation wears off, typically ready for discharge within 30-60 minutes. Due to sedation effects, patients must arrange transportation and avoid driving for 24 hours.
Conditions That Can Be Detected by Endoscopy
Endoscopy’s direct visualization capabilities enable detection of numerous conditions affecting the gastrointestinal tract that may be missed or inadequately characterized by external imaging or laboratory testing alone. This diagnostic precision makes endoscopy indispensable for accurate diagnosis and appropriate treatment planning.
GERD and Complications: Endoscopy detects esophagitis, erosions, strictures, and Barrett’s esophagus from chronic acid exposure.
Peptic Ulcer Disease: Gastric and duodenal ulcers are definitively identified, with biopsy distinguishing benign from malignant ulcerations.
Inflammatory Bowel Disease: Crohn’s disease and ulcerative colitis are diagnosed through characteristic inflammation patterns, ulcerations, and disease extent.
Celiac Disease: Upper endoscopy with small intestinal biopsies confirms celiac disease by demonstrating villous atrophy.
Polyps and Adenomas: Colonoscopy detects precancerous polyps that can be removed before progressing to cancer.
Infectious Colitis: Endoscopy with biopsies diagnoses infections including C. difficile colitis and parasitic infections.
Serious Conditions Which Can Be Detected by Endoscopy
Beyond routine inflammatory and benign conditions, endoscopy plays a critical role in detecting serious, potentially life-threatening pathologies requiring urgent intervention or intensive treatment. Early endoscopic detection of these conditions significantly impacts patient outcomes and survival.
Gastrointestinal Malignancies: Endoscopy with biopsy provides definitive diagnosis of esophageal, gastric, and colorectal cancers. Early detection through screening identifies cancers at curable stages.
Esophageal Varices: In cirrhosis patients, endoscopy detects enlarged esophageal veins at high rupture risk, enabling preventive treatment before life-threatening hemorrhage.
Advanced Barrett’s Esophagus with High-Grade Dysplasia: This precancerous condition requires intensive surveillance or treatment. Endoscopy detects dysplasia enabling intervention before cancer develops.
Acute Massive Hemorrhage: Endoscopy during active bleeding localizes hemorrhage sources and enables immediate hemostasis—potentially lifesaving interventions.
Ischemic Bowel: Endoscopy identifies ischemic colitis from compromised blood flow, guiding treatment decisions.

Possible Risks & Complications Involved in Endoscopy
While endoscopy is generally safe when performed by experienced gastroenterologists, patients should understand potential risks and complications associated with both upper and lower endoscopy procedures. Being informed enables patients to recognize warning signs requiring immediate medical attention after discharge.
Perforation: The most serious complication is perforation, creating a hole through the gastrointestinal wall. This occurs in approximately 1 in 1,000 to 1 in 2,500 colonoscopies. Symptoms include severe abdominal pain, fever, and rigidity requiring immediate surgical evaluation.
Bleeding: Post-procedure bleeding can occur after polyp removal or biopsy. Significant hemorrhage may require repeat endoscopy, blood transfusion, or rarely surgery.
Infection: While uncommon, infections including bacteremia or aspiration pneumonia can occur. Symptoms include fever, chills, or increasing abdominal pain.
Sedation-Related Complications: Adverse reactions to sedatives include respiratory depression, aspiration, or cardiovascular effects. Continuous monitoring minimizes these risks.
Cardiovascular Complications: Patients with heart disease may experience cardiac events during endoscopy triggered by procedural stress or sedation.

Side Effects of Endoscopy Test
Beyond serious complications, patients commonly experience minor side effects following endoscopy procedures.
Throat Discomfort: After upper endoscopy, mild sore throat or throat irritation is common, typically resolving within 24-48 hours.
Bloating and Gas: Air insufflation causes abdominal bloating and cramping that may persist for several hours. Walking helps expel retained gas.
Minor Rectal Bleeding: After colonoscopy with biopsies or polypectomy, small amounts of bright red blood in stool is expected for 1-2 days.
Drowsiness: Sedation effects persist for several hours, causing drowsiness and impaired judgment. Patients should avoid driving or operating machinery for 24 hours.

How to Prepare for an Endoscopy
Upper Endoscopy Preparation: Patients must fast for 6-8 hours before upper endoscopy to ensure an empty stomach. Most daily medications can be taken with small sips of water. Blood thinners may need temporary discontinuation depending on indication.
Lower Endoscopy Preparation: Colonoscopy requires thorough bowel cleansing. Dietary modifications start 2-3 days before with avoiding high-fiber foods. The day before, patients follow a clear liquid diet. Bowel preparation involves prescribed laxative solutions inducing diarrhea to empty the colon completely. Split-dose regimens provide superior cleansing.
General Preparation: Arranging transportation is mandatory as sedation prohibits driving. Patients should wear comfortable clothing and complete pre-procedure paperwork. Following all preparation instructions precisely maximizes procedural success and diagnostic accuracy.
Summary by Dr. Neelakanth Parappanavar
Throughout my years performing thousands of endoscopic procedures, endoscopy remains indispensable in gastroenterology—providing direct mucosal visualization, real-time tissue sampling, and immediate therapeutic intervention that external imaging cannot match.
Appropriate Indication Matters: Not every digestive symptom requires endoscopy. I carefully evaluate whether endoscopy will definitively answer clinical questions or enable therapeutic intervention. This judicious approach respects patient preferences and minimizes unnecessary risks.
Preparation Quality Determines Success: Excellent bowel preparation directly correlates with polyp detection rates. When patients struggle with preparation, I identify strategies—split-dosing, alternative regimens, anti-nausea medications, that improve compliance and diagnostic accuracy.
Communication Builds Trust: Comprehensive pre-procedure discussion addressing concerns, explaining expectations, and setting realistic goals significantly reduces anxiety and improves satisfaction. Taking time to listen builds therapeutic rapport.
Safety Is Paramount: While complications are rare, I instruct every patient about warning signs requiring immediate attention , severe pain, significant bleeding, fever and provide clear contact information. Most post-procedure symptoms represent expected side effects, but encouraging patients to call with questions prevents delayed complication recognition.
Addressing Common Concerns: Modern monitored sedation provides excellent comfort with remarkable safety. Upper endoscopy with appropriate sedation is virtually painless. Colonoscopy may cause temporary cramping, well-controlled with sedation. Post-procedure discomfort is generally mild and resolves quickly.
When I recommend endoscopy, patients can be confident that expected benefits substantially outweigh minimal risks, making it the appropriate next step in diagnostic evaluation or treatment. The temporary inconvenience pales compared to peace of mind from normal results or the life-saving potential of early disease detection.
Frequently Asked Questions About Endoscopy
Benefits of Endoscopy?
Accurate Diagnosis: Provides direct visualization of internal organs, revealing issues that imaging tests might miss.
Prevents Cancer: Removes precancerous polyps during colonoscopy before they become cancerous, reducing colorectal cancer risk by 76-90%.
Immediate Treatment: Allows doctors to treat problems during the same procedure—stop bleeding, remove polyps, dilate strictures, or extract foreign objects.
Minimally Invasive: Uses natural body openings instead of surgery, meaning faster recovery, less pain, and shorter hospital stays.
Tissue Sampling: Enables biopsies for definitive diagnosis of conditions like H. pylori, celiac disease, IBD, and cancer.
Cost-Effective: Prevents expensive surgeries and treats conditions before they become serious, reducing overall healthcare costs.
Is Endoscopy Painful?
No, endoscopy is generally not painful. Most procedures use conscious sedation (“twilight sedation”), which keeps you drowsy and comfortable with little to no memory of the procedure.
During Upper Endoscopy: You may feel brief pressure or gagging as the scope passes through your throat, but sedation minimizes awareness. Most patients don’t remember the procedure.
During Colonoscopy: You might experience mild cramping or pressure from air inflation, but sedation significantly reduces discomfort.
After the Procedure: Expect mild side effects like a sore throat (upper endoscopy) or bloating and gas (colonoscopy) that resolve within hours. These are uncomfortable but not painful.
Bottom Line: The anticipation is typically worse than the actual experience. With proper sedation, endoscopy is well-tolerated with minimal discomfort.
Can Endoscopy Detect Cancer?
Yes, endoscopy is highly effective at detecting gastrointestinal cancers including esophageal, gastric, and colorectal cancers.
How It Works: The camera allows direct visualization of suspicious areas—masses, ulcers, or abnormal tissue. When something looks concerning, immediate biopsy provides tissue samples for microscopic examination, confirming whether cancer is present.
Early Detection Saves Lives: Endoscopy finds cancers at early, highly treatable stages. Early-stage colorectal cancer has over 90% five-year survival compared to less than 15% for advanced disease.
Prevention Through Polyp Removal: Colonoscopy doesn’t just detect cancer—it prevents it by removing precancerous polyps before they turn malignant. This is why screening colonoscopy is so valuable.
Important Note: While highly effective, endoscopy requires tissue biopsy for definitive cancer diagnosis. Visual identification alone isn’t enough—pathological confirmation is essential.
What Not to Do After an Endoscopy?
Do Not Drive for 24 Hours: Sedation impairs judgment and reflexes even if you feel alert. Arrange a responsible adult to drive you home.
Do Not Make Important Decisions: Avoid signing contracts, making financial decisions, or conducting important business until the next day—sedation affects cognitive function.
Do Not Drink Alcohol: Combining alcohol with residual sedation can cause dangerous drowsiness and impaired breathing.
Do Not Ignore Warning Signs: Contact your doctor immediately if you experience:
- Severe or worsening abdominal pain
- Persistent vomiting or vomiting blood
- Fever or chills
- Heavy rectal bleeding
- Difficulty breathing or chest pain
- Severe throat pain or inability to swallow
Do Not Resume Blood Thinners Without Permission: Wait for your doctor’s specific instructions before restarting anticoagulants.
Do Not Exercise Strenuously: Avoid heavy lifting or intense workouts for the rest of the day. Light walking is fine and helps expel gas.
What You Should Do: Rest at home, start with light foods when permitted, stay hydrated, and walk periodically to reduce bloating. Most people feel normal within 24 hours and can resume regular activities the next day.