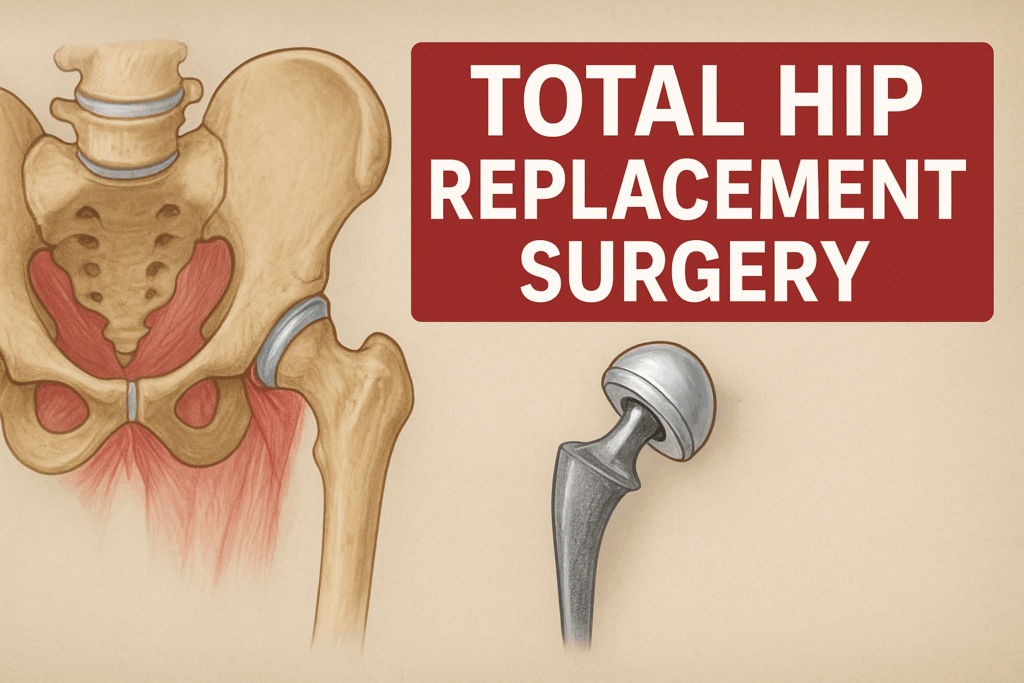
Total hip replacement, or Total Hip Arthroplasty (THA), is one of the most successful orthopedic surgeries in the world. This Surgical procedure is performed by removing the damaged parts of the hip joint, including both the acetabulum (socket) located in the pelvis and femoral head (ball) located in the upper end of femur.
Acetabulum & femoral head are replaced with artificial prosthetic components that mimic movements of a natural joint. The main objective of the procedure is to eliminate chronic hip pain, promote mobility, range of motion, and improve the overall quality of life, when non-surgical treatment methods have failed to provide relief to the patient.
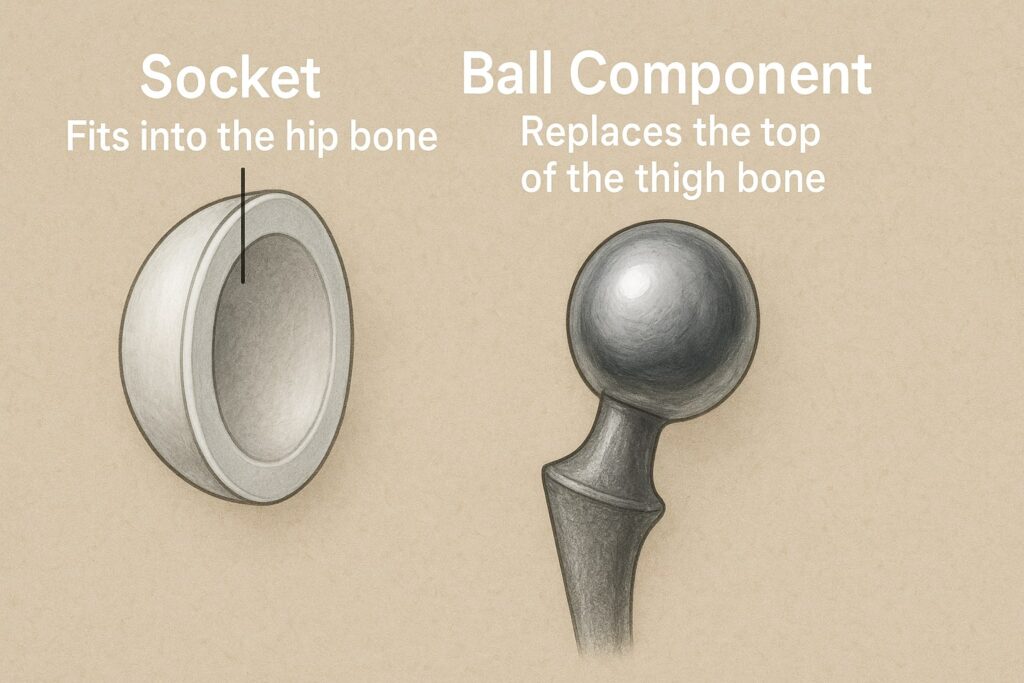
The artificial prosthetic consists of:
- A socket component: A metallic cup typically lined with a plastic (polythene) or ceramic liner and this component is installed into the pelvis’s acetabulum.
- A ball component: It consists of a ceramic or metal ball mounted on a metal stem and positioned into the femur (thigh bone).
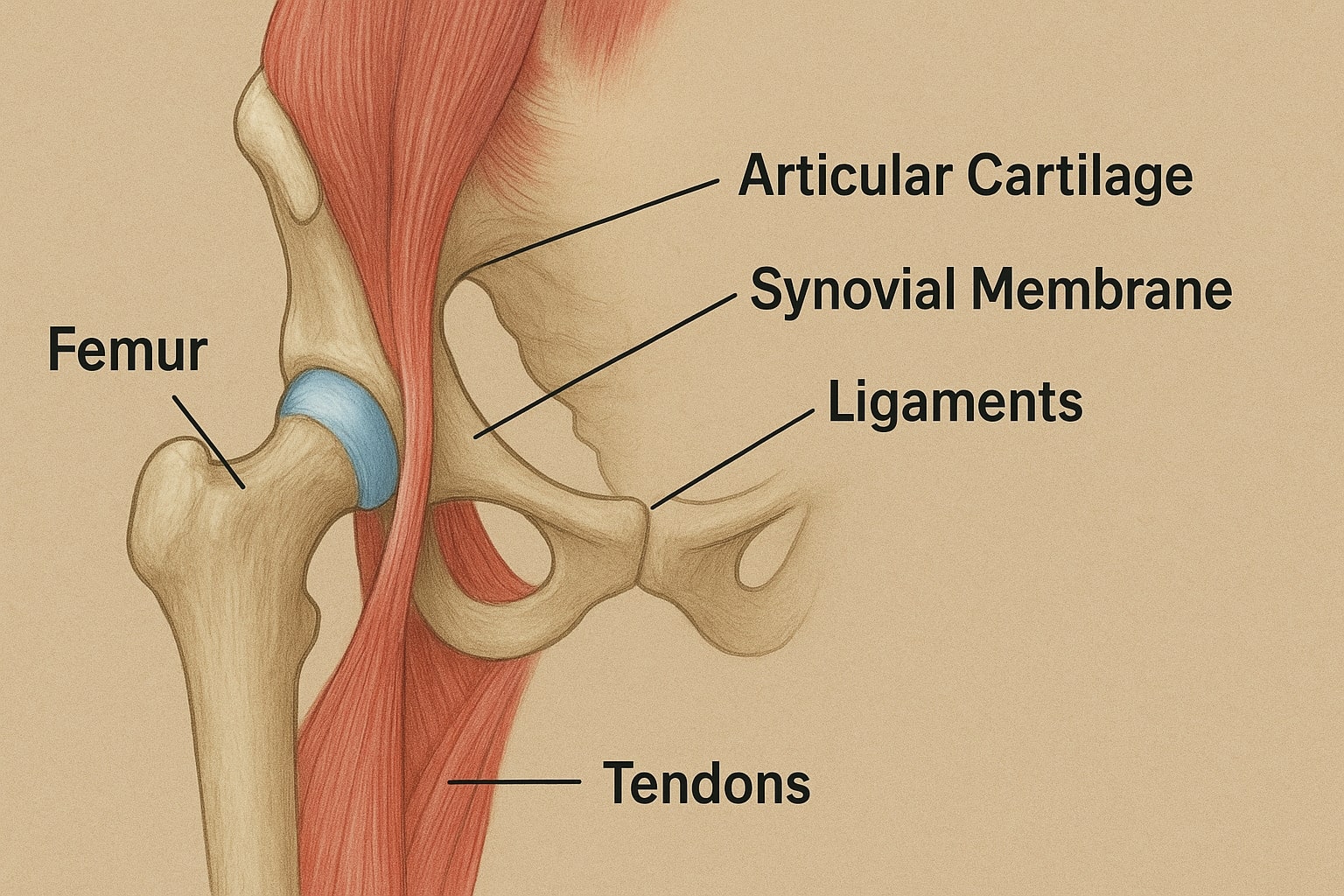
Hip Anatomy for Better Understanding
The hip is a ball and socket joint designed for mobility of a person, so we can walk, run and bend. Hip consists of:
- Femur (Thigh Bone): The femur is the longest and strongest bone in the human body. Its proximal part is a round knob known as the femoral head, which fits into an opening of another bone (the acetabulum) to move and support the weight of the body.
- Pelvis (Hip Bone): The pelvis includes a cup-shaped socket called the acetabulum which is the “socket” portion of the hip joint. This architecture houses the femoral head, to support smooth joint motion, stability or healthy wear and tear during daily activities.
- Articular Cartilage: The cartilage is a smooth, slippery coating that covers the bone surfaces of femoral head and acetabulum, wherein bones can slide easily with very little friction. When this cartilage gets damaged or worn, it is one of the primary causes of hip pain and limited motion.
- Synovial Membrane: A thin, fragile membrane that lines the joint and produces little amount of synovial fluid in order to lubricate the cartilage, minimize the friction, enable easy movement of the joints as well as support overall good health and function of a joint.
- Ligaments and Tendons: These are tough bands that hold the joint together by connecting bone to bone (ligaments) and muscle to bone (tendons). They offer stability along with controlled motion which allows normal and balanced movement in the joint.
Who is the Candidate for Total Hip Replacement Surgery?
The indication for total hip replacement is more influenced by the degree of pain and its functional implications rather than the age. However, the people aged between 50 to 80 years are more likely the candidate for hip replacement.
Whereas, orthopedic surgeons take patient symptoms, medical history, physical exam and x-ray findings into consideration on an individual basis to perform this procedure.
A patient is typically considered a candidate when:
- Nonsurgical treatments Failure: Non-surgical treatments like medicines (NSAIDs), physical therapy, corticosteroid injections and lifestyle changes.
- Pain is chronic and disabling: Severe pain that limits daily activities such as walking, climbing stairs and getting in or out of a chair.
- Persisting pain during rest: Even while the person is resting or sleeping, he/ she may suffer persisting pain making it uncomfortable to rest properly.
- Immobility: A person may lose mobility and feel stiffness and reduced range of motion impacting the quality of life.
- Radiographic evidence: There is evidence of a large amount of joint damage on X-ray, for example: some severe cartilage loss, bone spurs or substantial degenerative changes can be detected.
Conditions When Total Hip Replacement is Recommended
Most of the THA surgeries are performed to combat the pain and disability caused by certain hip problems. The surgery is recommended in the following medical conditions:
- Osteoarthritis (OA): This is the most common reason for a surgery. OA is a degenerative or “wear-and-tear” arthritis that happens when the protective cartilage on the ends of bones slowly breaks down over time.
- Rheumatoid Arthritis (RA): It is an inflammatory, autoimmune disease that attacks the synovial membrane, causing inflammation leading to severe pain as well as joint destruction.
- Post-traumatic Arthritis: This is a type of arthritis that can develop after traumatic injury to the hip caused mainly by a fracture or dislocation.
- Avascular Necrosis (AVN) or Osteonecrosis: It is a condition causing interruption in the blood supply to the femoral head temporarily or permanently, causing death of bone tissue and eventual collapse of the bone.
- Developmental Dysplasia of the Hip (DDH): A birth defect in which the ball and socket joint between the leg bone and pelvis is too shallow, causing it to become unstable and wear out early.
How to Prepare for Total Hip Replacement Surgery
Preparation is essential for a good surgery and recovery. It begins many weeks before the procedure itself, and it requires medical clearance, physical conditioning and logistical planning.
Methods of Preparations in Detail
1. Medical and Pre-Surgical Evaluation
- Primary Care Clearance: The orthopedic surgeon will need to clear that no existing conditions (e.g., heart disease, diabetes) are present. In case such conditions are present, they need to be stable prior to going into an operation.
- Diagnostic Tests: Essential diagnostic tests such as ECG (electrocardiogram) ,Blood tests and a chest X-ray are mandatory to evaluate the general health and suitability for anesthesia.
- Medication Review: Patients need to review all medications and supplements to the physician. Blood thinners (like aspirin, warfarin) frequently need to be stopped prior to surgery in an effort to reduce bleeding risks.
- Dental Examination: A dental check-up is needed to remove infections (like an abscess) because bacteria from an infected tooth can travel through the blood stream and enter a new hip joint.
2. Physical and Home Preparation
- Pre-Surgery Exercises (Pre-habilitation): Pre-surgery exercises to help strengthen the muscles around the hip and upper body can be prescribed by a physical therapist. Before surgery, being more physically fit can dramatically speed up post-operative recovery.
- Weight Management: If a person is overweight, in that case reducing as little as three to eight percent of a body weight can take the pressure off the joint which helps in eliminating a surgical risk.
- Home Safety Modifications: It is necessary to prepare the home according to the needs for early recovery when mobility is limited. Safety modifications can be done in following ways:
- Safety equipment such as a shower stool, higher toilet seat and handrails must be installed in the bathroom.
- Set up a recovery area on the top or ground floor to cut down on stair usage.
- keep essential items like phone, remote, books, medications near to you.
3. Logistical and Social Planning
- Post-Surgery Support: It’s important to have a family member available for a few weeks after discharge, who can assist in tasks like cooking, shopping and transportation etc.
- Rehabilitation Planning: It’s also important to determine where patients will undergo their post-hospital rehabilitation process (e.g., inpatient rehabilitation facility, skilled nursing, or outpatient physical therapy).
How Long Does Total Hip Replacement Surgery Take?
The operating room time for Primary Total Hip Replacement Surgery is 1 to 2 hours long but the whole process from pre-operative care to post-operative care takes longer time.
- Pre-operative Time (1-2 hours): This process involves registering into the surgical center, consultation with the anesthesiologist and surgical team, preparing the patient (IV lines, monitoring devices), and induction of anesthesia.
- Surgical Time (1-2 hours): At this time the surgeon makes an incision and removes the affected joint components to prepare for the new prosthetic joint and closing the incision.
- Post-Anesthesia Care Unit (PACU) Time (1-3 hours): After the surgery, the patient is transferred to a recovery room and immediate monitoring of vital signs is done as the effects of the anesthesia wear off. This is the point at which the pain management process begins.
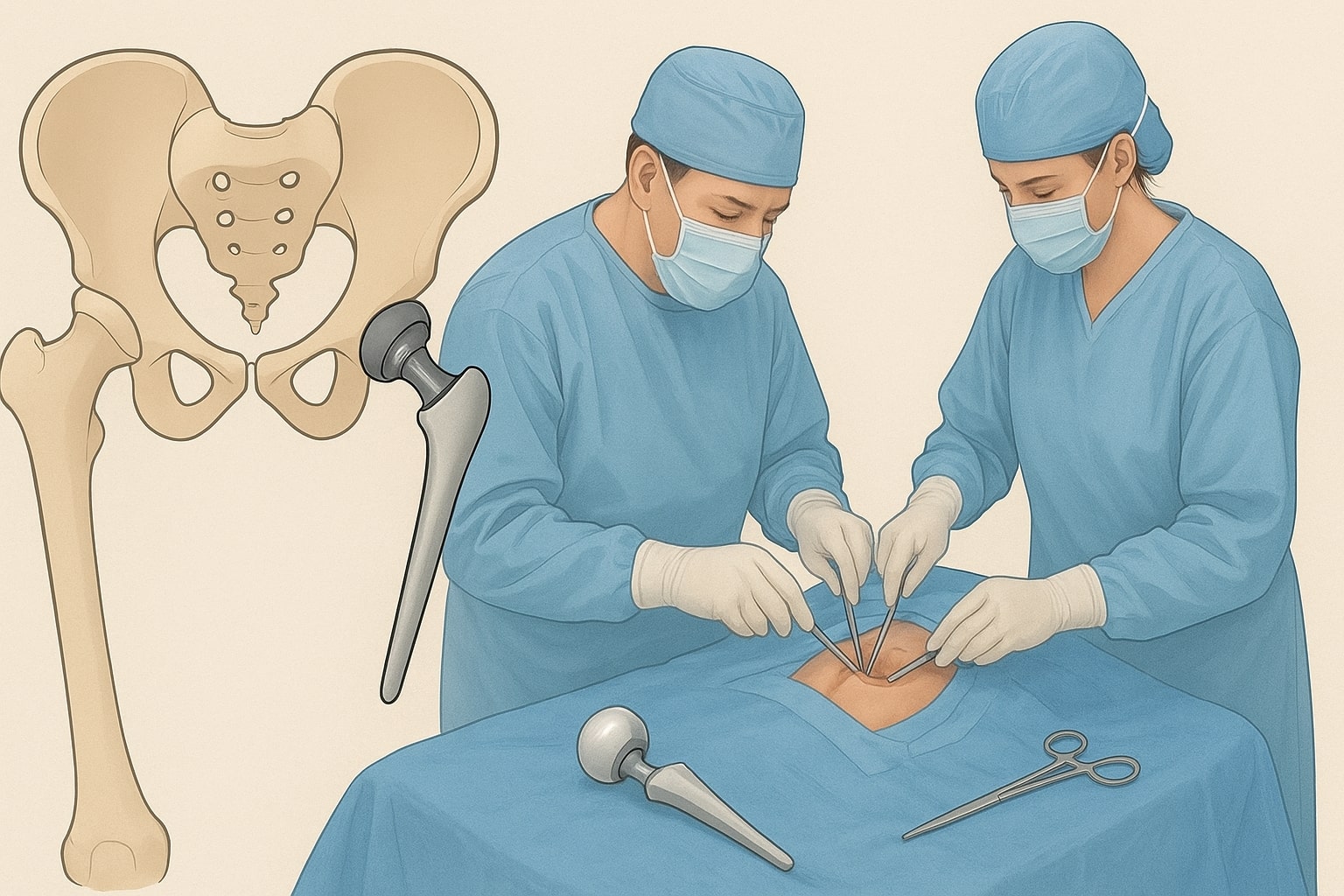
Total Hip Replacement Surgery Steps
The total hip replacement is a very technical surgical procedure done under perfect and sterile conditions. Certain steps differ slightly depending on the method of surgery (e.g., posterior, anterior or lateral), however the basic concept of replacing the defective ball and socket is always the same.
The Surgical Procedure: A Basic Overview
The procedure is fundamentally about accessing the hip joint, removing the arthritic or damaged bone and cartilage, preparing the remaining bone to accept the implant, and securing the prosthetic components. The key is to achieve a stable, smooth-moving joint that is correctly sized to restore leg length and joint mechanics.
Fundamentally, the operation involves gaining access to the hip joint, taking out arthritic or damaged bone and cartilage, shaping the remaining bones to make a way for an implant and putting both pieces in place. The challenge lies in obtaining stable, smooth articulating joints that are of the appropriate size in order to restore leg length and joint mechanics.
The Steps in Detail
1. Anesthesia and Incision
- Anesthesia: The patient is given general anesthesia which makes them sleep throughout the procedure, or regional anesthesia (like a spinal or epidural block) along with sedation.
- Incision: The surgeon will make an incision (usually 6-10 inches, sometimes smaller for a minimally invasive procedure) to open the hip joint. The exact site of incision is determined by the surgical approach employed.
2. Accessing and Dislocating the Joint
- Muscle and Tissue Management: Once the hip joint is clearly exposed, the muscles and soft tissues around the hip can then be cautiously shifted or gently parted. This step enables the surgeon to visualize all of joint structures along with preventing undesired damage to surrounding tissues, ensuring accurate surgical intervention.
- Joint Dislocation: the femoral head is smoothly moved proximally out of the acetabulum, which is then empty. This intentional dislocation permits the surgeon a clear view and access to both femoral and acetabular surfaces which facilitate precise debridement of diseased tissues and preparation for prosthetic placement.
3. Preparing the Acetabulum (Socket)
- Femoral Head Removal: The femoral head (the ball part of the hip joint) is removed from the neck of the thighbone, or femur. This step enables the segmental damaged bone to be removed and the site is prepared for prosthesis implant.
- Reaming: Special instruments (called reamers) are used to remove the damaged cartilage and bone from inside of the acetabulum, which is then prepared as a hemispherical socket with surgical implants.
- Socket Insertion: The replacement socket (acetabular component) is inserted into the bone cavity prepared for it, then a liner made of either plastic or ceramic is snapped in place in the shell. The shell may be held in the bone with screws.
4. Preparing the Femur (Ball)
- Femoral Canal Preparation: Sizing and alignment of the femoral intramedullary canal are carefully reamed and shaped. This preparation allows the prosthetic stem to obtain tight fitting in the canal with stability and best load transfer after implantation.
- Stem Insertion: The artificial metal stem is fitted into the femur’s hollow shaft so there will be tight fit. It may be press fitted to support natural bone ingrowth, or cemented in place with orthopedic cement for immediate and secure fixation.
- Ball Attachment: The metal or ceramic new femoral head is then fixed onto the top of the stem. It is a replacement for the natural ball of the hip joint with smooth movement in the socket restoring function and stability to the joint.
5. Reduction and Closure
- Reduction: The new artificial ball is then inserted into the newly-drilled socket and adjusted by the surgeon to fit. This realignment re-establishes the normal movement of the hip joint, providing smooth rotation and enhanced stability as well as an improved overall function of the joint.
- Checking Stability: The leg is carefully controlled with different movements to ensure the new hip joint is stable, well aligned and moves freely. This step is also useful in determining that the leg length is properly balanced and equal.
- Wound Closure: Once the procedure is finished, the incision is carefully closed or stapled in multilayers to encourage healing. A dressing is placed to cover the operative wound and protect it from infection.
Total Hip Replacement Surgery Complications
Although THA is a very successful surgery like all other surgeries, there are potential risks and complications involved in the procedure. The risk of more severe complications is small (usually under 2%), but patients should be informed about this risk. Major surgery complications include:
- Infection: The wound or the area around the prosthesis can become infected. It is treated with antibiotics, and in severe cases further surgery may be necessary. Preventatively, off-site sterilization and post-surgical sterile treatment are provided.
- Blood Clots (Deep Vein Thrombosis – DVT): There are high chances of clot formation in leg veins. If a piece of that clot breaks loose and goes to the lung (Pulmonary Embolism – PE), it can be fatal. Prevention includes blood thinners, compression stockings and early mobilization.
- Dislocation: The new ball can come out of the socket. This risk is highest in the first few weeks after surgery and often requires a closed reduction (re-positioning without surgery). Specific hip precautions are implemented to prevent this.
- Nerve and Blood Vessel Injury: Rare but possible complications include injury to nearby nerves and blood vessels that can surround the hip joint when surgery is being performed. This may cause temporary or partial weakness, numbness, or bleeding. Careful surgical approach and modern imaging can effectively reduce this risk.
- Difference in Leg Length: Even with accurate surgical planning, slight differences in leg length may result following surgery. Surgeons aim for perfect alignment but there’s a margin of errors. In some case people need to wear shoe lifts or undergo physical therapy in order to feel comfortable walking.
- Loosening or Wear: Sometimes the artificial parts of a joint can become loose or the plastic cushion between the two joints can wear out from use. This can be painful or unstable and may result in a revision surgery to replace the worn components.
- Fracture: Patients with weaker bones are at risk of a ruptured bone either during surgery or after surgery. According to the severity of the break, treatment can include surgical stabilization with screws or plates or even removal and replacement of an implant in severe cases.

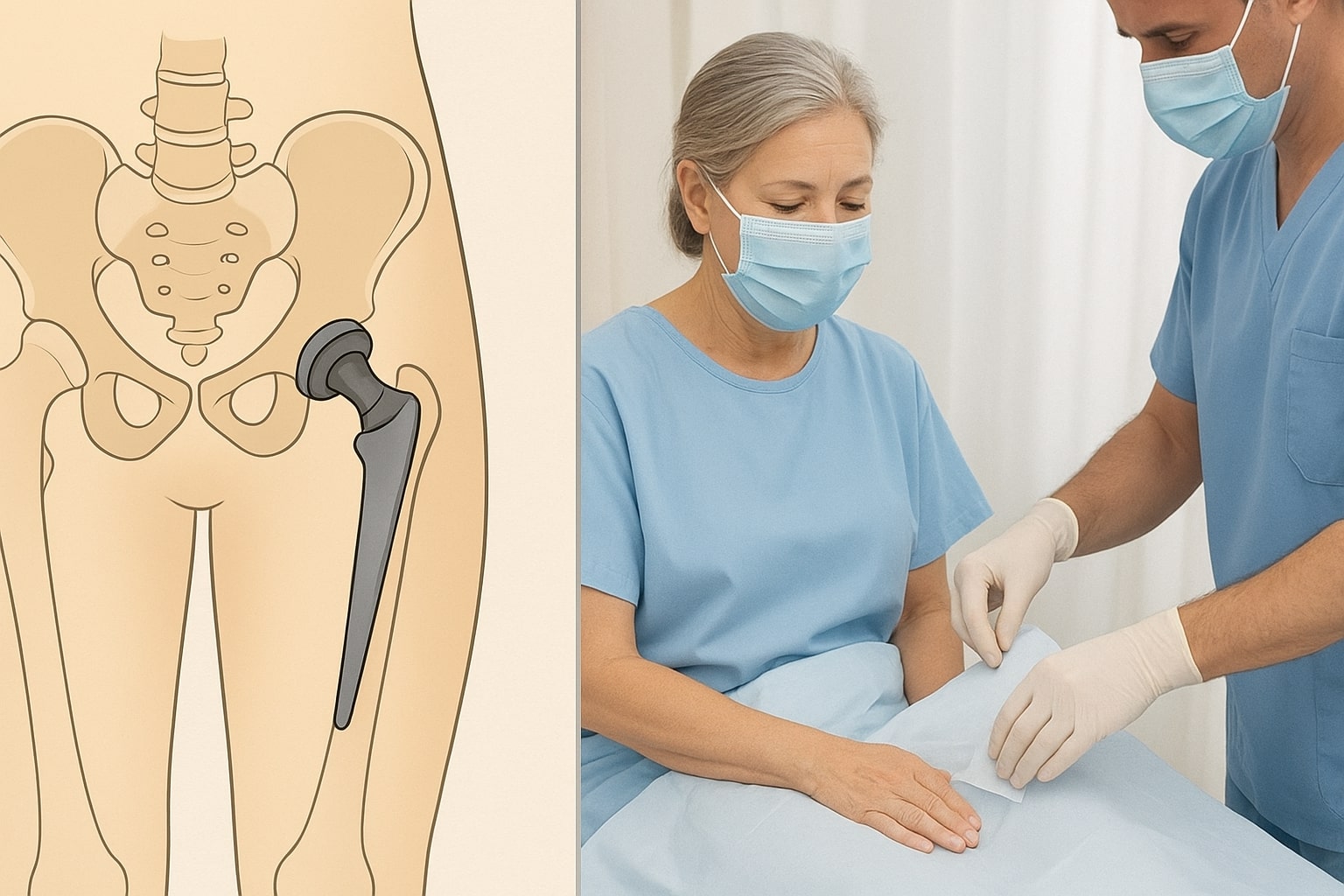
Total Hip Replacement Surgery Recovery Time
Recovery is a defined process that commences right after surgery and continues for many months in several phases.
Hospital Stay (1-3 days):
- The patient is encouraged to stand and walk with assistance (walker or crutches) often within 24 hours of the surgery.
- Physical therapy begins immediately, focusing on safe mobilization, transfer techniques, and adhering to hip precautions.
Initial Home Recovery (Weeks 1-6):
- This is the most crucial phase. The patient focuses on pain management, increasing walking distance, and intensive physical therapy, typically 3-5 times a week.
- Dependence on walking aids lessens, and the ability to perform basic daily activities improves significantly. Most non-strenuous activities are resumed.
Intermediate Recovery (Weeks 7-12):
- The patient usually switches from a walker or crutches to a cane or no aid at all.
- Focus shifts to regaining strength and a more normal gait (walking pattern). Most driving is often resumed around 4-6 weeks, pending surgeon approval and the patient’s ability to safely operate pedals.
Full Recovery (3-6 Months and Beyond):
- While the surgical wound heals quickly, muscle and tissue strength restoration takes the longest. A full recovery, where a patient feels largely unrestricted in routine activities and non-impact sports, typically takes 6 months to one year.
Success Rate of Total Hip Replacement Surgery
Total Hip Replacement Surgery has an outstanding track record, consistently ranking among the most successful procedures in modern medicine.
- Survival Rate of Implants: The success rate is measured by the longevity of the implant. Currently, data shows that over 90-95% of modern hip replacements are still functioning well 10 years after surgery, and over 80-85% are still successful at 20 years.
- Functional Success: Success is also measured by the patient’s subjective relief. The vast majority of patients report a dramatic reduction or complete elimination of hip pain, leading to a significant improvement in mobility and quality of life.
Expert Advice: Why You Can Trust Modern Hip Surgery
It is entirely understandable for a patient facing major surgery to feel panic or anxiety. However, the patient must understand that orthopedic implant technology and surgical techniques have advanced exponentially over the last few decades. Modern total hip arthroplasty is performed with highly specialized, durable materials (metal alloys, ceramics, and advanced polyethylene) and precision-guided instrumentation.
Furthermore, the focus has shifted toward rapid recovery protocols (ERAS – Enhanced Recovery After Surgery), which drastically reduce hospital stays, minimize narcotic use, and prioritize immediate mobilization. This means the procedure you are considering is safer, more precise, and comes with a more predictable and faster recovery trajectory than procedures performed even 10 or 15 years ago. Trust the established data and the experienced surgical team.
Lifestyle After Total Hip Replacement Surgery
The new hip is designed for durability, but certain modifications can ensure its longevity and prevent complications.
- Safe Activities: Patients are encouraged to pursue low-impact activities like swimming, cycling, golf, walking, and ballroom dancing.
- Activities to Avoid: High-impact sports that involve running, jumping, or contact (e.g., jogging, football, basketball) should generally be avoided as they increase the risk of implant wear and loosening.
- Hip Precautions: Depending on the surgical approach, specific hip precautions (e.g., avoiding deep bending past 90 degrees, avoiding crossing the legs) may need to be followed indefinitely or for a defined period to prevent dislocation.
- Dental Care: Prophylactic antibiotics are often recommended before any major dental work (like extractions) to prevent bacteremia (bacteria in the blood) from traveling to and infecting the implant.
Post-Surgery Care and Diet Plan
Successful recovery heavily relies on diligent post-operative care and optimal nutrition.
Post-Surgery Care:
- Wound Care: Keep the incision clean and dry. Report any signs of infection immediately (increased redness, warmth, discharge, fever).
- Pain Management: Follow the prescribed pain medication regimen. Transition from narcotic pain relievers to over-the-counter pain relievers (like acetaminophen) as soon as possible.
- Physical Therapy (PT) Adherence: Consistent and dedicated attendance to PT sessions and home exercises is non-negotiable for regaining strength, range of motion, and a normal gait.
Diet Plan:
- Protein: Crucial for wound healing and muscle repair. Focus on lean meats, poultry, fish, eggs, and legumes.
- Fiber: Important to prevent constipation, a common side effect of pain medication and reduced mobility. Increase intake of whole grains, fruits, and vegetables.
- Hydration: Drink plenty of water (8-10 glasses per day) to support healing and maintain proper blood flow, aiding in DVT prevention.
- Calcium and Vitamin D: Essential for bone health, especially if the implant is uncemented, allowing bone to grow onto the surface.