Diabetes mellitus is a long-term condition. It affects how the body processes blood sugar, also known as glucose. Diabetes is now a common health issue. It can also lead to other serious problems like heart disease, stroke, kidney failure, and nerve damage.
Type 1 and Type 2 diabetes are the most prevalent forms of diabetes. Although both relate to insulin, the causes, progression, management, and prevention of each differ substantially.
This guide explains the differences between Type 1 and Type 2 diabetes. It covers their causes, symptoms, and how to treat, prevent, and manage them.
What is Type 1 Diabetes Mellitus?
Type 1 diabetes is an autoimmune disease. In this condition, the immune system attacks and destroys the beta cells in the pancreas that make insulin. People with this disorder cannot produce insulin. Insulin is a hormone that helps move glucose from the blood to the body’s cells for energy.
Since insulin is essential for life, people with Type 1 diabetes need insulin treatment for the rest of their lives.
Doctors usually diagnose it in children, adolescents, and young adults, so they sometimes call it juvenile-onset diabetes. But it can strike at any age.
Key Characteristics of Type 1 Diabetes:
- Rapid onset
- Absolute insulin deficiency
- Requires lifelong insulin replacement
- Not preventable
- Linked to autoimmunity
Prevalence:
While less prevalent than Type 2 diabetes, Type 1 diabetes impacts between 5-10% of all people with diabetes worldwide.

What is the Main Cause of Type 1 Diabetes?
The precise etiology of Type 1 diabetes is not yet completely known. Nevertheless, experts commonly consider the disease to result from an autoimmune assault caused by genetic and environmental factors.
Potential causes and risk factors include:
Autoimmune Reaction : The body’s immune system errantly attacks insulin-producing beta cells in the pancreas.
Genetics : A family history of Type 1 diabetes or other autoimmune conditions may also elevate the risk. Researchers associate some of the genes, such as HLA‐DR3 and HLA‐DR4, with greater risk.
Viral Infections : Viruses like Coxsackievirus, mumps, and rubella can trigger immune reactions in people who are genetically prone to them.
Geography and Ethnicity : Type 1 diabetes is more common in people of European descent. It is also more common in those from countries farther from the equator.
Important Note: Unlike Type 2 diabetes, lifestyle factors do not cause Type 1 diabetes.

Symptoms and Effects of Type 1 Diabetes Mellitus
Symptoms and effects of type 1 diabetes can show up quickly. They can be life-threatening if not treated right away.
Common Symptoms:
- Excessive thirst (polydipsia)
- Frequent urination (polyuria)
- Rapid and unexplained weight loss
- Constant hunger
- Fatigue and drowsiness
- Irritability and mood swings
- Blurred vision
Severe Effects and Complications:
Untreated Type 1 diabetes can lead to diabetic ketoacidosis (DKA). This is a serious condition. It happens when the body lacks insulin. Without insulin, the body’s cells cannot get glucose. As a result, the body starts breaking down fat for energy.
Long-term complications include:
- Cardiovascular disease
- Kidney damage (nephropathy)
- Eye damage (retinopathy)
- Nerve damage (neuropathy)
- Problems with the feet because of improper blood flow
What is the Meaning of Type 2 Diabetes Mellitus?
Type 2 diabetes is a metabolic disease. It is marked by insulin resistance. This means the body does not use insulin well. As a result, the pancreas makes less insulin. Over time, this leads to poor blood sugar control.
Unlike Type 1, people with Type 2 diabetes still make insulin. However, their cells do not respond to it well.
This type of diabetes develops slowly. It is usually found in people over 40. However, it is becoming more common in young people and children. This change is due to poor diets and a lack of exercise.
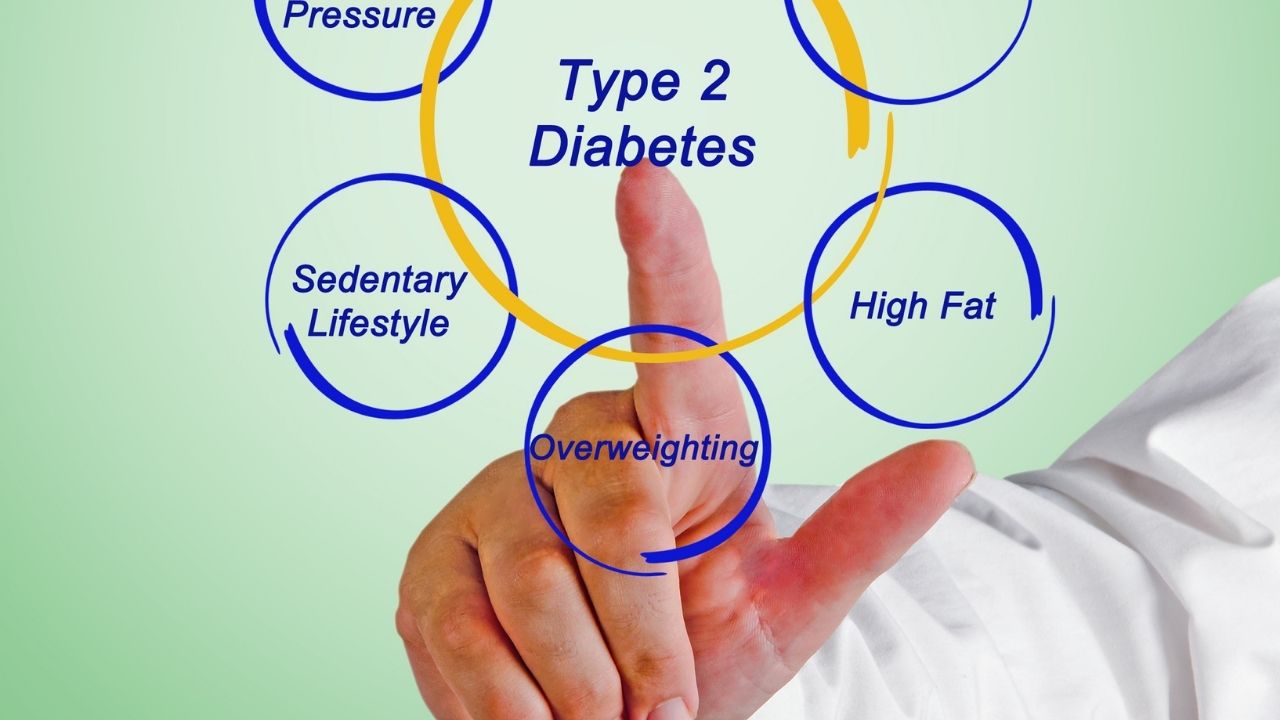
What is the Main Cause of Type 2 Diabetes?
Type 2 diabetes starts and progresses due to a mix of genetic factors and lifestyle choices.
Common Causes and Risk Factors:
- Insulin Resistance: Muscles, fat and liver cells become resistant to insulin and glucose does not get taken up well.
- Obesity and Overweight: One of the prime contributors is excess body fat, notably abdominal fat.
- Physical Inactivity: It promotes weight gain and insulin insensitivity, an expression of the metabolic syndrome.
- Unhealthy Diet: This risk is higher when sugar, processed foods and saturated fats are consumed in large quantities.
- Genetics and Family History: Those with a first-degree relative who has, or had, Type 2 diabetes are at greater risk.
- Age and Ethnicity: The latter risk rises with age, particularly after 45. Minority groups including South Asians, African Americans and Hispanics are more at risk.
What are the Symptoms of Type 2 Diabetes Mellitus?
Symptoms of Type 2 diabetes can be very mild. You might not notice them at all. Sometimes, people do not show any symptoms. This can make it easy to blame stress or tiredness and ignore the problem.
Common Symptoms:
- Increased thirst
- Frequent urination
- Constant hunger
- Slow wound healing
- Fatigue
- Blurred vision
- Tingling or numbness in hands or feet
- Recurrent infections, especially of the gums, skin, or vagina.
Long-term Effects:
If poorly managed, Type 2 diabetes can lead to:
- Cardiovascular diseases
- Kidney failure
- Vision loss
- Amputations due to foot ulcers
- Neuropathy
Key Differences Between Type 1 and Type 2 Diabetes
| Factor | Type 1 Diabetes Mellitus | Type 2 Diabetes Mellitus |
| Nature | Autoimmune disease | Metabolic disorder |
| Insulin production | Absent or minimal | Present but not effective |
| Onset | Rapid onset, usually in children or young adults | Gradual onset, typically in adults |
| Body Type | Often lean or underweight | Frequently overweight or obese |
| Symptoms appearance | Sudden | Gradual |
| Ketoacidosis risk | High risk | Rare |
| Family history relevance | Less prominent | Strongly linked |
| Prevention possible? | No | Yes, often through lifestyle |
| Initial treatment | Insulin injections or pump | Diet, exercise, oral meds, possibly insulin |
| Lifestyle relation | Not related to lifestyle | Strongly related to diet, activity, and weight |

Treatment of Diabetes Mellitus Type 1 and 2
Treatment for Type 1 Diabetes:
No cure exists for type 1 diabetes, but the condition can be managed in the following ways:
- Insulin Therapy: Needs daily insulin shots or treatment with an insulin pump.
- Blood Glucose Monitoring: Glucometer or continuous glucose monitor (CGM) with frequent checking (4–10 times a day).
- Carbohydrate Counting: Balancing carb intake to match insulin doses.
- Healthy Diet: Meals that are balanced to keep blood sugar levels normal.
- Regular Exercise: Increases sensitivity to insulin and health in general.
- Education and Support: Diabetes education and mental health programs.
Treatment for Type 2 Diabetes:
Type 2 diabetes can sometimes be reversed or put into remission. This is more likely if it is diagnosed early. Treatment options include:
Treatment options include:
1. Lifestyle Modifications such as:
Weight loss
Well balanced diet (low in sugar, high in fiber)
30 minutes of exercise daily
2. Oral Medications:
Metformin is commonly prescribed.
Other classes are SGLT2 inhibitors, DPP-4 inhibitors, and sulfonylureas.
3. Insulin (if needed):
Administered when oral medications are not adequate.
4. Monitoring Blood Glucose:
Frequent monitoring to evaluate dietary and drug effects.

Prevention and Management of Diabetes
Preventing Type 1 Diabetes:
At present, there is no way to prevent Type 1 diabetes. Research is still happening to create vaccines or immune therapies. These treatments aim to stop the autoimmune attack, but they are not available to everyone yet.
Preventing Type 2 Diabetes:
Type 2 diabetes can often be prevented through:
- Regular physical activity
- Healthy eating habits
- Maintaining healthy weight
- Quitting smoking
- Controlling blood pressure and cholesterol
- Regular screening if you are at high risk
Managing Both Types of Diabetes:
Regardless of the type of diabetes, effective diabetes management involves:
- Strict blood sugar control
- Medication adherence
- Regular check-ups
- Eye, kidney, foot and dental checks
- Support for mental health and to reduce stress
- Patient education programs
Summary
Knowing the difference between Type 1 and Type 2 diabetes is important. This knowledge helps with early detection, proper treatment, and living a healthy life. While each condition has problems with insulin and blood sugar, they have different causes. They affect different ages and need different treatments.
- Type 1 diabetes is an autoimmune disease that necessitates lifelong insulin treatment and monitoring.
- Type 2 diabetes often comes from unhealthy lifestyle choices. You can manage it and sometimes reverse it. Weight loss, a healthy diet, and regular exercise can help. You may also need certain medications.
Whether you have diabetes or are at risk for it, there is a secrets like early detection, the right lifestyle, and good medical care. You can live a healthy and productive life, even if you have diabetes. You just need the right information and support.





