Cardiac disease (also known as heart disease or CVD, cardiovascular disease) refers to a range of many diseases that impact how the heart and blood vessels function. It is one of the biggest public health challenges globally, claiming millions of lives a year. These conditions may involve the heart muscle, valves, arteries, veins or electrical conduction system of the heart.
And at its core, cardiovascular disease impairs the heart and circulatory system’s ability to properly deliver blood, oxygen and nutrients to tissues and organs. Its dysfunction crowned the complexity of the network ,capable of generating life-threatening sequelae as severe as myocardial infarction (heart attack), stroke, heart failure, even sudden cardiac death.
According to World Health Organization (WHO) cardiovascular disease is actually the leading cause of death globally, responsible for around 32% of all global deaths per year. A lot of these deaths can be prevented with early detection, lifestyle changes, and prompt medical treatment.
In short, knowledge of what cardiac disease is, its mechanisms, its risk factors, and its management,can help put control of your heart health in your hands, and lessen long term complications.
What Causes Cardiovascular Disease
Cardiovascular disease (CVD) is typically the end result of a convergence of modifiable and non-modifiable risk factors. Genetics and age are factors, but most causes arise from lifestyle and environmental exposure.
1. Atherosclerosis – The True Culprit
Atherosclerosis is the most frequent underlying mechanism in the context of cardiovascular disease. It is a chronic inflammatory process that results in the build-up of lipid-rich atheromatous plaques in the vessel wall. Over time these plaques harden and narrow the arteries, restricting blood flow and increasing the potential for clotting.
2. High Blood Pressure (Hypertension)
Hypertension is often referred to as the “silent killer” as it slowly but surely affects the walls of arteries from the inside, making them less elastic and prone to blocking. Hypertension’s constant force against arteries substantially increases the risk for a heart attack, stroke and heart failure.
3. Dyslipidemia (Increased Lipid Levels)
So other than the fateful best practice which is blamed directly at atherosclerosis, other dozens of contributive factors are high density lipoprotein (LDL) “bad” cholesterol and low density lipoprotein (LDL) “good” cholesterol. When combined with other metabolic diseases, high triglycerides further complicate the situation.
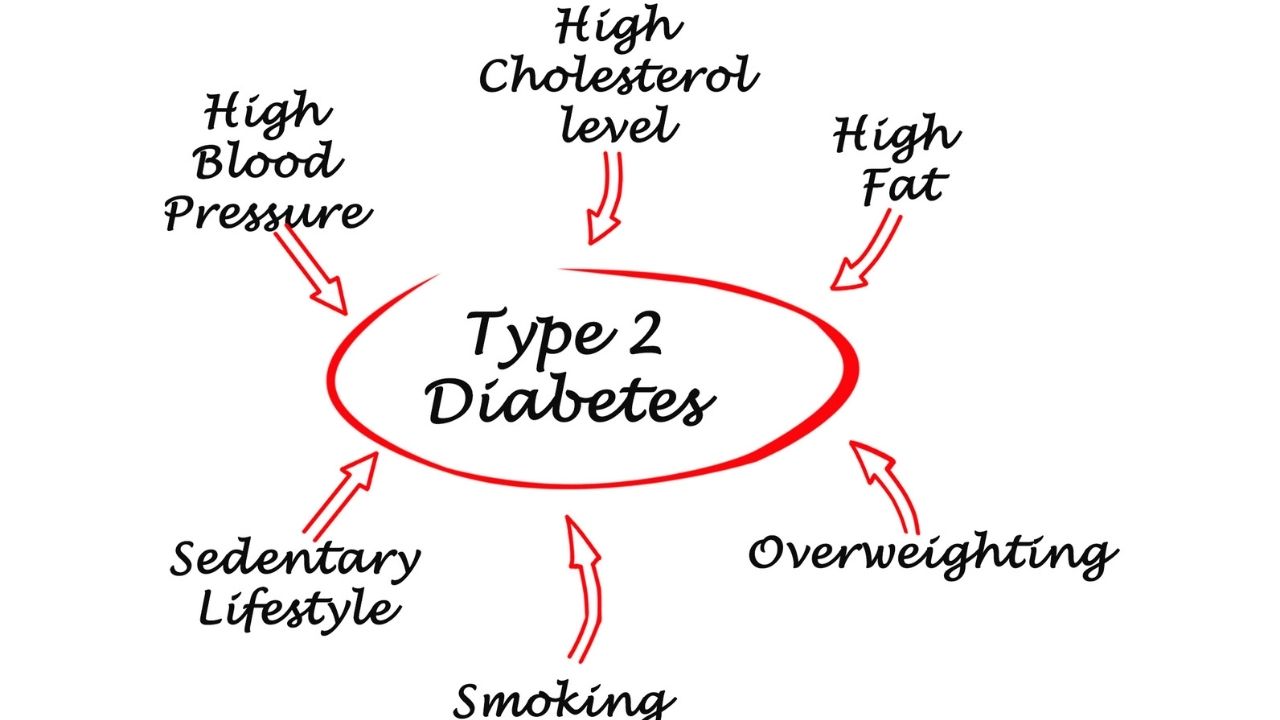
4. Diabetes and Insulin Resistance
People with type 2 diabetes or prediabetes have elevated blood glucose levels that cause vascular damage and have a higher risk of nerve damage. People with diabetes tend to have an earlier and more severe manifestation of heart disease.
5.Cigarette and Tobacco Smoking
The impact of tobacco use is multifactorial, it exerts toxic effects to the endothelial lining of blood vessels, promotes hypercoagulability, decreases oxygen availability and promotes atherosclerosis formation. Compared to a non-smoker, a smoker is 2 – 4 times more likely to develop heart disease.
6. Diabetes and Obesity Along with Sedentary Lifestyle
Visceral fat accumulation is linked with increasing insulin resistance, hypertension, atherogenic dyslipidemia, and inflammation. Then complicating all of these risk factors is a sedentary lifestyle.
7.Poor Nutritional Habits
Diets rich in processed foods, saturated and trans fats, excess sodium and added sugars lead to endothelial dysfunction and systemic inflammation that worsens lethargy of heart disease.
8. Alcohol Consumption
Although moderate alcohol may provide some minimal cardiovascular protection in certain populations, heavy or binge drinking raises blood pressure, causes irregular heart rhythms and may cause cardiomyopathy.
9. Influence of chronic stress on mental health
Stress impacts the cardiovascular system directly ,with changes to hormones and indirectly by inducing unhealthy habits, like overeating, drinking and smoking. Conditions of mental health such as depression and anxiety have become established as cardiovascular risk factors.
10. Genetic Predisposition
A family history of early heart disease (before age 55 in men, 65 in women) signals a genetic factor. Genetic mutations may also predispose to lipid disorders, arrhythmias or structural abnormalities.
Recognizing these varied causes paves the way for early intervention, risk reduction and lifetime heart health management.

What Are the Different Types of Heart Disease
Heart disease is an umbrella term that encompasses a number of conditions that affect the different parts of the cardiovascular system. Understanding these differences can help inform diagnosis, treatment and long-term management. Different types of heart diseases include:
1. Coronary Artery Disease (CAD)
This is the most common type and occurs when the coronary arteries become narrow or blocked in response to plaque buildup, limiting the circulation of oxygen to the heart muscle. Coronary artery disease (CAD) causes myocardial infarction, angina and sudden cardiac death.
2. Heart Failure (HF)
Heart failure doesn’t mean the heart isn’t beating, it means it’s not pumping blood efficiently. CAD, hypertension, cardiomyopathy. Symptoms may include fatigue, shortness of breath and fluid retention, and reduced ability to exercise.
3. Arrhythmias
These are abnormal heart rhythm. Common types include:
Atrial fibrillation (AFib) : the most common type, which increases stroke risk.
Ventricular tachycardia (VT) : a rhythm that can be deadly.
Bradycardia : extremely slow heartbeat. Others can cause palpitations, dizziness, fainting or sudden death.
4. Valvular Heart Disease
This is the most common type and happens when the coronary arteries narrow or block due to plaque buildup, restricting the flow of oxygen to the heart muscle. Coronary artery disease (CAD) is the cause of myocardial infarction, angina and sudden cardiac death.
5. Congenital Heart Defects
These are congenital structural abnormalities. They include everything from simple congenital conditions like atrial septal defects to complex malformations requiring surgical correction. Others may not show symptoms until they reach adulthood.
6. Cardiomyopathy
This is a disease of the heart muscle, which can be:
- (Enlarged (dilated) chambers, weak pumping)
- Hypertrophic (thickened walls, often genotype)
- Restrictive (thickened walls, restricted filling) Cardiomyopathies may result in arrhythmias or heart failure.
7. Pericardial Diseases
The pericardium ( a double-walled sac surrounding the heart ) can become inflamed (pericarditis), fill with fluid (pericardial effusion) or stiffen (constrictive pericarditis) all of these affect heart function.
8. Peripheral Arterial Disease (PAD)
While primarily affecting the limbs, PAD is an important marker of systemic atherosclerosis and a strong predictor of future heart attack or stroke.

What Are the Signs of Heart Disease
Prompt recognition of early symptoms of heart disease, however, can significantly improve prognosis through timely intervention. But the signs can differ, depending on age, gender and type of heart disease.
Common Warning Signs:
Chest pain or discomfort: A classic symptom, usually brought on by physical activity or stress, and relieved by rest. It might even feel like pressure, squeezing, burning or fullness.
Shortness of breath: Happens with exertion or when lying flat. May suggest heart failure or CAD.
Palpitations : Feeling a fluttering or pounding in your chest, often a symptom of arrhythmias.
Fatigue or weakness: A common symptom of heart failure or progressive CAD, one that occurs more often when simple tasks are tiring.
Dizziness or fainting: Related to low cardiac output or irregular heart rhythms.
Swelling in legs, ankles, or abdomen: Resulting from fluid buildup in heart failure.
Cold sweats, nausea and lightheadedness: These may occur during a heart attack, particularly in women or older adults.
Chronic cough or wheezing: Particularly at night or when lying down, this can be a sneaky sign of heart failure.
Bluish lip or fingertips: Little to no oxygen circulating, which could be due to congenital defects or severe heart failure.

Atypical Symptoms in Women:
Women may report:
- Unusual fatigue
- Jaw, neck, or upper back pain
- Indigestion or heartburn
- Symptoms resembling anxiety or panic attacks
Being familiar with both classic and atypical presentations is critical to prevent missed or delayed diagnosis.

Is Heart Disease a Chronic Disease
Yes, heart disease is categorically considered a chronic disease. It usually progresses slowly over many years, often without any clear symptoms until extensive damage has been done.
Here are some characteristics of chronic illness.
Long-term changes: Diseases such as CAD, heart failure, and arrhythmias take years to develop.
Chronic treatment demand: Management requires short-term drug treatment along with lifestyle changes and frequent follow-up.
Potential for worsening: At any phase, acute events can happen like heart attacks or sudden worsening of symptoms.
Impact on quality of life: Can hinder physical capacity, psychological health, and daily function.
Heart disease is another chronic disease, and should be managed like other chronic diseases, such as diabetes, chronic kidney disease (CKD) or chronic obstructive pulmonary disease (COPD). The aim is to manage progression, minimize symptoms, and improve survival.
How Can Heart Disease Be Treated
Heart disease treatment is a holistic, multidisciplinary approach, addressing the root causes and comorbidities.
1. Lifestyle Modification
Lifestyle Modification is the basis of heart disease treatment. It include:
- Heart-healthy diet: A focus on fruits, vegetables, legumes, lean proteins, and healthy fats. Reducing salt, sugar, red meat and processed foods.
- Exercise: A minimum of 150 minutes week of moderate-intensity aerobic exercise.
- Weight control: Maintaining a healthy body mass index improves both blood pressure and lipid levels, as well as insulin sensitivity.
- Tobacco cessation: Quitting tobacco smoking is a key component of lowering cardiovascular risk.
- Stress reduction: Mindfulness, yoga, and sufficient sleep hygiene.

2. Pharmacological Management
Treatment varies depending on the specific form of heart disease:
Antihypertensives: ACEIs, ARBs, Ca-channel blockers and beta-blockers
Statins: The cholesterol-controlling drugs
Antiplatelets : Inhibit clotting in vulnerable patients.
Diuretics: woozy fluids in heart failure
Antiarrhythmics: Regulate or prevent abnormal heart rhythms.
Anticoagulants: Reduces strokes in diseases such as atrial fibrillation
3. Surgical and Other Interventional Procedures
When medication isn’t enough then following measures are taken:
Percutaneous coronary intervention (PCI): Angioplasty with stenting.
Coronary artery bypass grafting (CABG): For multi-vessel disease.
Valve repair or replacement : For faulty heart valves.
Implanted devices: Pacemaker, defibrillators, and ventricular assist devices.
4. Cardiac Rehabilitation
Supervised programs of exercise, education and counseling to assist patients in recovery and avoid subsequent cardiac events.
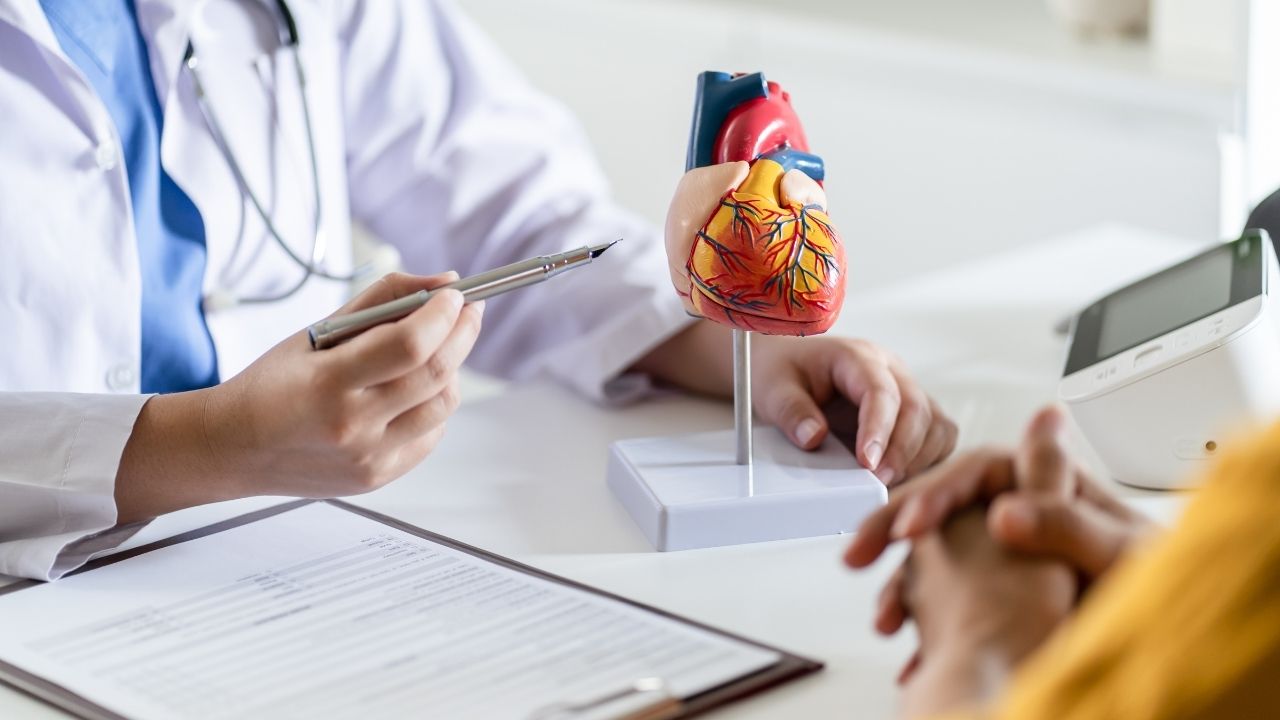
5. Regular Monitoring
Will need lifelong follow-up with cardiologists. Tools include:
Echocardiograms
Stress tests
Electrocardiograms (ECGs)
Blood tests
Holter monitoring
Final Thoughts
Having knowledge of what cardiac disease is, its causes, types, symptoms and treatments is not just an academic exercise, it is a matter of life and death. Cardiovascular disease is a chronic, often progressive disease, and thus, a preventive approach is needed.
Although the diagnosis brings about changes that affect lifestyle, medical therapy and chronic care are coveted parts of having a chronic illness; with them, human beings can live longer and healthier. Raising awareness about this and improving access to care and adopting heart-healthy habits will be crucial as we efforts to change this global burden of cardiovascular disease.
Summary
Cardiac disease, or cardiovascular disease (CVD), is a term for a wide range of conditions affecting the heart and blood vessels and is one of the biggest threats to global health in the world today. These conditions from coronary artery disease and arrhythmias to heart failure can develop insidiously over decades, spurred by unhealthy lifestyle habits, inherited risk and underlying conditions such as diabetes or hypertension. Underlying causes of cardiovascular disease often include high blood pressure, smoking, obesity, poor diet and sedentary lifestyle.
Awareness of these types of heart disease, alongside congenital heart defects, heart infections and cardiomyopathy, can aid early recognition and treatment. Characteristic signs of heart disease are chest pain, shortness of breath, fatigue, and abnormal heartbeat, but symptoms would depend on the kind and severity of disease. Heart disease is a chronic disease, and like all chronic diseases, it requires lifelong control with medication, lifestyle adjustments, and regular medical attention.
For one, lifestyle modification and medication to interventional procedures like angioplasty or even surgery, there are many treatment options available. With early identification and ideal treatment, cardiac illness is controllable, and individuals can stay energetic, fulfilling lives. Awareness and prevention are still the most important tools to stop its global spread.